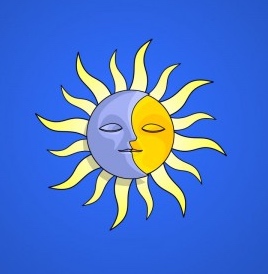
Vitamin D is known as the Sunshine vitamin. This is because 90 percent of our vitamin D requirements naturally comes from the sun. Bioavailable vitamin D3 is created in the skin through the action of the sun’s UV-B rays on cholesterol (7-dehydroxycholesterol), as one of five forms.
Vitamin D is known as the Sunshine vitamin. This is because 90 percent of our vitamin D requirements naturally comes from the sun. Bioavailable vitamin D3 is created in the skin through the action of the sun’s UV-B rays on cholesterol (7-dehydroxycholesterol), as one of five forms.
Diet offers the remaining ten percent in fish liver oils, fatty fish, egg yolks, and as fortified foods, as both Vitamin D2 and D3. These forms are not biologically active. Vitamin D2, added to “D-fortified foods,” is produced synthetically by exposing the mold ergot (ergosterol) to ultraviolet light. This process was patented and licensed to pharmaceutical companies which is used as prescription vitamin D. D4 and D5 are synthetic analogues of D3 being tested in vitro for the treatment of cancer and heart disease. To date, Harvard research reports that vitamin D supplementation does not result in a lower incidence of cancer or cardiovascular events than placebo.
Even so, vitamin D’s reputation as a potent cancer fighter has been mainstream news for at least a decade. A lack of vitamin D is also reported to be behind increased rates of infections, stroke, diabetes, osteoporosis, and autoimmune disorders. Models and articles have most of us convinced that excess vitamin D intake could reduce cancer deaths by 75 percent. Why else would the government add vitamin D2 to fortify food? Meanwhile, as cancer rates rise, we are urged to cover up with sunscreen against the sun which nature intended as the truest source of vitamin D. Why the contradiction?[1]
Vitamin D Misunderstood
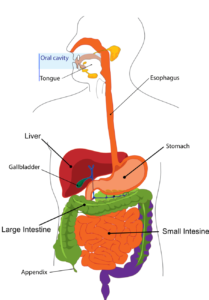
Much of the research, to date, conceptualizes vitamin D as a resource which gets used up and must be replenished through supplementation – like supplying gasoline to a car. However, this assumes vitamin D acts like a vitamin when in fact it is a secosteroid hormone (cholecalcipherol) that functions like other steroid hormones, such as cortisol and testosterone. Fro the blood, vitamin D3 is converted to its active form by two hydroxylations:
- the first conversion is in the liver to become 25(OH)D (calcidiol), the inactive, primary storage hormone. This is the most abundant circulating form and is therefore the most common measure of serum levels by the medical community primarily because active D3 has a short half-life, so is not considered a reliable measurement of vitamin D.
- the second conversion is in the kidneys to form 1,25(OH)2D (calcitriol), mediated by the parathyroid hormone. This 1,25-D active form binds to vitamin D-binding protein, a carrier protein in the plasma before going to the vitamin D receptor (VDR) on target cells to activate important functions such as calcium absorption in the intestines, phosphorous metabolism, and the activation of the innate and adaptive immune systems. In addition to the kidneys, calcitriol is also synthesized by monocyte–macrophages in the immune system. When synthesized by monocyte-macrophages, calcitriol acts locally as a cytokine, defending the body against microbial invaders by stimulating the innate immune system.
The real story on Vitamin D has shifted, even if its translation in the press and in practice has been slow. Evidence now clearly shows that the assumption that low D levels cause inflammatory diseases is flat out wrong. Rather, when we see vitamin D in its true light, it is as a marker and a consequence of the inflammatory disease process. Thus, if the liver is congested, or “fatty,” and if parathyroid hormone levels are high, it makes sense that vitamin D levels in the blood would be low, as a 2013 study in India shows.
The alternative hypothesis is a game changer and deserves its own headline. So it is no surprise that going a step further, to say that vitamin D supplementation can potentially exacerbate disease proliferation, might challenge even the most open-minded practitioners.
The Alternative Hypothesis
One of the great mysteries in human biology is the fact that most human breast milk is considered deficient in vitamin D. Yet why would Nature overlook such an important nutrient in the “perfect food?”
 Case in point: when lactating mothers take all but exceedingly high levels of vitamin D – 6,000 IU which is 15 times the United States Recommended Daily Intake – the vitamin D content in breast milk remains low.[2]
Case in point: when lactating mothers take all but exceedingly high levels of vitamin D – 6,000 IU which is 15 times the United States Recommended Daily Intake – the vitamin D content in breast milk remains low.[2]
The medical community measures inactive 25-D as “healthy “ for children and adults within a serum level between 20-40 ng/ml. Some consider a level between 50-80 ng/ml to be optimal. Suggested daily doses range from 4,000 iu and as high as 50,000 iu for short periods in order to reach “optimal” (30-80 ng/L) serum levels.
- Sufficient: 20–30 ng/mL, or 50–75 nmol/L
- Safe upper limit: 60 ng/mL, or 150 nmol/L
- Toxic: above 150 ng/mL, or 375 nmol/L
The (medical) jury is still out on what an optimal serum 25-D level should be.
If vitamin D levels differ within the body, do they also differ among cultures?
Since before 2012, studies have showed widespread D-deficiency among Asian Indians. In a 2003 study, researchers postulated that a group considered to be “healthy” hospital workers must have sufficient D levels from their exposure to the sun. However, when results showed that only 34% had 25-D concentrations above 15 ng/ml and 20 percent had levels below 5 ng/ml, (well below the 30-80 ng/ml range) researchers deemed the entire staff as “deficient.”[2.5] A 2012 updated study showed the same results. Other research in south India shows that exposure to sunlight between the hours of 11 a.m. and 2 p.m. will promote vitamin D production in the skin year round. In the tropics, that equates to a latitude 13.40° N and longitude 77.2° E, from May 2007 to August.
The authors of the Indian studies did not consider an alternative hypothesis. They did not question that “healthy” from one measure (inactive 25-D) may not tell the whole story. They didn’t consider that their “normal range” might be unnaturally adjusted upward to accommodate the high levels of consumption of fortified D-products in the West. Neither did they question the fact that secosteroids work differently from vitamins, or that cultural differences, themselves, might account for the differences in hormones.
Further studies showed similar “low 25-D” status in African Americans when compared with Eastern Europeans. Mainstream science says that low 25-D in African Americans and other groups with dark skin results primarily because pigmentation reduces vitamin D production in the skin. Current beliefs suggest “healthy African Americans do not achieve optimal (inactive) 25D concentrations at any time of year.” However, the study showed that “healthy blacks” are indeed healthy when considering levels of D-binding protein and other hormones. When looking at the broader picture, concentrations of bioavailable 25-D are similar between blacks and whites based on differences in genetic polymorphisms[3] and environmental variables.[4] An updated study between black and white Americans shows similar results.
Some Keys to D-Activation
 1.Vitamin D Receptor (VDR)
1.Vitamin D Receptor (VDR)
As a secosteroid, vitamin D is controlled by multiple delicate feedback pathways through the vitamin D receptor (VDR). The VDR is the heart of the innate immune system at the site of each cell, responsible for the expression and regulation of 2000 genes, turning up the expression of some, turning down the expression of others. Under most conditions, the active 1,25-D form acts as the “on” switch to activate the VDR and immunity, while the inactive form acts as the “off” switch. 25-D is not completely inactive, but it cannot activate the VDR. According to Trevor Marshall, author of The Marshall Protocol, not only does the inactive 25-D inactivate VDR, but so does supplemented vitamin D which can go on to suppress innate immunity.
2. Melanin
Melanin in the skin affects the synthesis of vitamin D through specialized cells called melanocytes, located at the base of the epidermis by specialized cells called melanocytes. These cells have photosensitive receptors, similar to those in the eye that detect UV radiation from the sun and other sources. Within a few hours of UV exposure, melanin is produced as the number and size of melanin granules increase.
More than a sun shield, not only does melanin reduce the chances of skin cancer, but it also helps preserve the body’s supply of folate which prevents the risk of miscarriage and babies with neural tube defects. (Too much UV may cause the breakdown of folate). Because folate is required for DNA replication in dividing cells, its absence has an affect on many processes in the body. Hormonal changes during pregnancy stimulate the production of melanin as seen by darkened skin (i.e., linea nigra).
Melanin is a key to life because it is present in both sperm and egg and supervises the growth of the developing fetus. It is present at the inception of life, and needed for reproduction. Melanocytes resemble nerve cells and are essential for transferring energy. Lack of or insufficient melanin in the embryo causes the mother to lose her baby.
2. Prolactin
The production of active 1,25-D is also increased by prolactin, a hormone which stimulates lactogenesis (the formation of milk in mammary glands), which requires large amounts of calcium. Prolactin also acts like a cytokine by binding to cytokine-like receptors and is, therefore, an important regulator of the immune system.
Why does most reporting on vitamin D fail to connect the dots that lead to the vital force of the healing sun? Could it be that the Vitamin D Council is driving vitamin D science to suit its own agenda even while the concept of vitamin D “deficiency” is rapidly becoming obsolete? In fortifying the food chain with unnatural vitamin D, we have fooled with Mother Nature and come to the point where we no longer know what the body’s natural level of vitamin D is.
Could “D-deficient” really be “D-sufficient?”
The Truth About “D”
In cases when whole populations are given large amounts of vitamin D, the only ones who remain “deficient” appear to be those whose immune systems are fighting disease. Could these people be actively downregulating active vitamin D in favor of the inactive form? Could low vitamin D levels be a biomarker for other imbalances?
“Homeostatic regulation” means that hormones such as 25-D work in cooperation with other hormones, substrates, ligands, enzymes, bacteria, minerals, receptor sites, energy, etc. Like any hormone, it has both an active and an inactive form, in order to up-regulate or down-regulate the immune system to adapt to its environment. The website, Chronicillnessrecovery.org writes that chronic disease is “multifactorial with many pleomorphic, intracellular species involved. The various species can work in concert and may have even mutated specifically for the host by sharing genetic information by horizontal transfer of DNA.”
 Part II: The Two Faces of Vitamin D
Part II: The Two Faces of Vitamin D
Studies show the action of vitamin D to be biphasic, with a stimulatory effect at lower concentrations, and becoming more inhibitory or ineffective at higher levels. In the same way autoimmune disease responds to corticosteroid (Prednisone) treatment, vitamin D can temporarily reduce symptoms of disease, but long-term use appears to dramatically increase the odds of disease relapse.
For example, when excess D is supplemented, cells respond by reducing the number of receptors, thereby downregulating the system, or alternatively cells become more receptive to the inactive form of the hormone. If there is a shortfall of vitamin D, the cells will increase the number of receptors, thereby upregulating the system and become more sensitive to the uptake of active hormone. In the case of vitamin D, supplementing with too much active D may actually suppress the immune system as levels of the inactive form increase.
A Self-regulating Model
Vitamin D action is complex, but also intuitive. In light of contradictory evidence and shifting views, science should never ignore the alternative hypothesis. Science must question the answers. Instead of rationalizing the data it is high time to reexamine the model.[5]
The true model of the vitamin D feedback system is self-regulating. A self-regulating system monitors itself; no outside assistance necessary. When the VDR receptor is activated, it transcribes the gene (CYP24A1) for the P450 enzyme that inactivates 1,25-D. This downregulation maintains homeostasis to limit the concentration of 1,25-D to just that amount needed for proper transcriptional activation of the VDR.
When excess 25 D is taken in through supplementation, high levels of D can disrupt natural communication in the feedback system by allowing the creation of unrequested active 1,25D. Active vitamin D, in the presence of no open VDR receptors, binds to other receptors: such as the thyroid, cortisol, and testosterone receptors to create hormonal imbalances. Enzymes in tumor cells can work overtime to break down vitamin D to limit survival in cancer cases.
When observing patients with autoimmune disease, inactive 25-D, lacking one hydroxyl group, can block the VDR gene. Researcher, Paul Albert in his article Vitamin D: the alternative hypothesis, says [5.5]:
Researchers are recommending vitamin D supplementation at historically unprecedented levels. Yet, by most measures, rates of chronic diseases that ought to be reduced by such supplementation continue to escalate. A reconsideration of the deficiency/disease model is warranted. The alternative model is based on the growing possibility that persistent bacteria drive autoimmune disease.
Under such circumstances, 25-D, which inactivates the VDR, palliates symptoms over the short-term, but allows chronic pathogens to proliferate over time. If so, low 25-D in patients with autoimmune diagnoses is the result, rather than cause, of the disease process – further undermining any therapeutic benefit from vitamin D supplementation.
According to researcher Trevor G Marshall, inactive “25-D levels are naturally downregulated by the disease process itself – a process driven by the ability of chronic, intracellular metagenomic pathogens to create VDR-blocking ligands.”[6]
In a study by Joyce Waterhouse, “lower average levels of vitamin D frequently observed in autoimmune disease are not a sign of deficiency. Instead, it is proposed that the lower levels result from chronic infection (known as Th1 illnesses) with intracellular bacteria (known as Th1 pathogens) that dysregulate vitamin D metabolism by causing vitamin D receptor (VDR) dysfunction within phagocytes.”[7]
Why are women diagnosed with 78% of autoimmune disease? According to the the August 2014 issue of Frontiers in Neuroenocrinology, gender differences may play a main role:
- women produce stronger humoral and cellular immune responses to antigen than males (Ansar Ahmed et al., 1985).females produce higher levels of CD4 + T cells in response to immunization (Ho et al., 1995).
- women produce higher levels of circulating antibodies than men (Rowley and Mackay, 1969), which could underlie their propensity to produce higher levels of autoantibodies in autoimmune diseases (Whitacre et al., 1999).
- women show increased immune reactivity (Hewagama et al., 2009), and this greater immunocompetence may translate to greater resilience to infectious and some non-infectious diseases. However, it is possible that this greater immune reactivity makes women more prone to developing autoimmune disease (Zandman-Goddard et al., 2007).
Got Leaky Gut?
 We are 10:1 more bug than human cells. We are microbiome (bacteria) with at least 10% virome (virus/exosome), yeast and parasites. Our microbiota evolves right along with us. In high numbers, they produce ligands that bind and inactivate the gene (VDR) which encodes the nuclear receptor for vitamin D3. It is through our microbes and their byproducts that humans derive disease and health.
We are 10:1 more bug than human cells. We are microbiome (bacteria) with at least 10% virome (virus/exosome), yeast and parasites. Our microbiota evolves right along with us. In high numbers, they produce ligands that bind and inactivate the gene (VDR) which encodes the nuclear receptor for vitamin D3. It is through our microbes and their byproducts that humans derive disease and health.
VDR is found in all immune cells all over the body. When ligands from pathogens bind to the VDR gene, they downregulate active vitamin D and block its transcription for more. Opportunistic bacteria, yeast, and fungus, and their toxic byproducts (biotoxins), create an environment that benefits them. And why not? They are merely responding to their environment based on our choices. In return, our cells respond by releasing cytokines that cause inflammation, which under chronic conditions, can lead to tears in the lining of the small intestine, which can lead to “leaky gut” and autoimmunity. Inflammation of the gut penetrates the brain through the gut-brain axis to cause “leaky brain.” A cascade reaction begins as chronic inflammation snowballs and expands to affect organ systems and pathways. To the outside observer, it appears that one autoimmune disease snowballs into others.
Like us, our microbes survive to thrive. They live under the law of Pleomorphism whereby if the conditions of the terrain (microbiome) change, so do they. As shapeshifters, they adapt and reproduce as we do.
Therefore, building gut integrity to close the gaps can restore innate immunity for the host. Innate immunity is made up of your mucosal epithelia, which includes skin, airway, reproductive tract, interstitium, and intestine. The mucosa and intersitium are the main interface between us and our microbial world, both pathogenic and symbiotic microbes. At this level communication are natural defenses, including the gut associated lymphoid tissues, with Peyer’s Patches, T-cells, macrophages, neutrophils, etc. Heal the gut? Heal the immune system.
Even in light of new evidence, the beauty of sun-loving, self-sustaining vitamin D continues to be ignored by the mainstream. So the concept of vitamin D “deficiency” continues unabated by medical and natural doctors, alike, who push vitamin D supplementation without addressing the true cause. And disease statistics escalate. It’s clear that this trend can only be remedied by a rise in independent thinking.
Part III: The Studies
For half a century, medical science has been noting the association between Vitamin D serum levels and disease. What developed has been a concept of ‘Vitamin D Deficiency’ based solely on the assumption that ‘low’ Vitamin D serum levels somehow cause disease processes. But this ignores the alternate hypothesis — that the disease processes themselves regulate the Vitamin D metabolism — that the observed ‘low’ values of Vitamin D in disease are a result of the disease process, and not the cause. – Article, Vitamin D Discovery Outpaces FDA Decision Making
Vitamin D and Yeast Infection
One of vitamin D’s roles is to produce an anti-microbial peptide called cathelicidin, a critical component in the lysosomes of macrophages, in leukocytes, and in keratinocytes to fight off bacterial infection, as well as Candida (yeast). VDR also transcribes TLR2, needed for macrophages to detect an internal infection, within themselves.
For example, sarcoidosis is an inflammatory disease that infects the phagocytes of the immune system. It has a bacterial pathogenesis.[8] More specifically, it is a cytoplasmic microbiota of intraphagocytic, L-form bacteria that seems to drive the biochemical changes observed in sarcoidosis, because it responds to antibiotics.[9] Therefore, reversing bacteria-induced D-receptor dysfunction is key for sarcoidosis and all autoimmune disease.[10] A number of autoimmune diseases can be reversed by gradually restoring VDR function with the VDR agonists which, from the medical community, have included certain bacteriostatic antibiotics. Trevor Marshall, the author of the Marshall Protocol, developed this protocol to heal his own sarcoidosis.
When it comes to vitamin D metabolism, the body relies on its own wisdom, the innate immune system. “When the immune system is challenged by injury or pathogens, TGF-beta and/or interferon-gamma are released, additional CYP27B1 is generated, and thus additional (active) 1,25-D In turn, the VDR is activated to express more antimicrobial peptides (cathelicidin and beta-Defensin-2). Additionally, when the VDR is activated, TLR2 is expressed, allowing the immune system to recognize gram-positive bacteria, including Staphylococcus aureus, Chlamydia pneumonia, and Mycoplasma pneumoniae.”
A study published in the August 2015 issue of the Journal of Infectious Diseases found both a positive and negative relationship between different doses of vitamin D and Candida infection. In mice, low doses of activated vitamin D reduced fungal burden and led to improved survival compared to mice not given activated vitamin D. However, high doses of activated vitamin D led to poor outcomes in the mice. Researchers concluded, “Mechanistically, low dose (activated vitamin D) induced proinflammatory immune responses. These beneficial effects were negated with higher vitamin D doses.”[11]
Vitamin D and Cardiovascular Disease
A 2013 study in the American Journal of Cardiology found an inverse relationship between vitamin D and C-Reactive Protein (a factor linked to stiffening of the blood vessels and increased risk of artherosclerosis). Researchers concluded, “The inflammation that was curtailed by vitamin D does not appear to be curtailed at higher levels of vitamin D.” “The inverse relation between vitamin D supplementation and inflammatory biomarkers among asymptomatic adults is not settled.”[12]
“Clearly vitamin D is important for heart health, especially if you have low blood levels of vitamin D. It reduces cardiovascular inflammation and atherosclerosis, and may reduce mortality, but it appears that at some point it can be too much of a good thing.” Study leader Muhammad Amer advised caution in supplementation. “Those pills could have unforeseen consequences to health even if they are not technically toxic.” Note: Each 100 international unit of vitamin D ingested daily produces about a one nanogram per milliliter increase 25-Hydroxyvitamin D levels in the blood.
In the February 2014 issue of the Journal of Endo. Met. a similar relationship was found between activated D and homocysteine levels with a positive relationship when vitamin D stayed below 21 ng/L and a negative relationship above 21 ng/L. Hyperhomocysteinemia is an independent risk factor for premature atherosclerosis and thromboembolism.[13]
Again, we see that increasing levels of the active form 1,25-D do not always solve an inflammatory problem. Like Nature, everything strives for balance while interacting with its environment, including vitamin D steroid hormone.
Recall that researchers have made similar misjudgments regarding the relationship between cholesterol and heart disease, only in reverse. When looking at the broader picture, it becomes clear that cholesterol (like 1,25-D) is a biomarker, not a cause of disease. Cholesterol protects against atherosclerosis and infections. People with high cholesterol (not low) actually live longer.
Vitamin D And Osteoporosis
Active 1,25-D increases blood calcium levels by increasing the uptake of calcium from the gut into the blood. So high serum levels of vitamin D absolutely require higher levels of calcium. When dietary sources of calcium are exhausted the body takes it from the bone, resulting in osteoporosis. This process exhausts the telomeres that create the osteoclasts and osteoblasts constantly required to maintain these high D levels.
 Extra calcium can precipitate in arteries and on the outside of the bones, causing arteriosclerosis and bone-deformities. It can also settle in joints and ligaments, and can cause muscle-cramps because the blood-calcium level needs to be low enough to deport calcium from muscle cells. It can also kill muscles cells (if the calcium cannot be deported), eventually causing fibromyalgia. Might the high serum levels of Ca (from supplementation) explain the calcification diseases seen today? Like other chronic diseases, osteoporosis is often accompanied with a very low vitamin D level. Instead, the body may require more boron, magnesium, and other minerals to come into balance.
Extra calcium can precipitate in arteries and on the outside of the bones, causing arteriosclerosis and bone-deformities. It can also settle in joints and ligaments, and can cause muscle-cramps because the blood-calcium level needs to be low enough to deport calcium from muscle cells. It can also kill muscles cells (if the calcium cannot be deported), eventually causing fibromyalgia. Might the high serum levels of Ca (from supplementation) explain the calcification diseases seen today? Like other chronic diseases, osteoporosis is often accompanied with a very low vitamin D level. Instead, the body may require more boron, magnesium, and other minerals to come into balance.
Longterm vitamin D supplementation can result in an increased risk of hypercalcemia, the most common life-threatening metabolic disorder associated with neoplastic diseases, occurring in an estimated 10% to 20% of all adults with cancer. Solid tumors (such as lung or breast cancer tumors) as well as certain hematologic malignancies, particularly multiple myeloma, are most frequently associated with hypercalcemia.[14]
Primary hyperparathyroidism is the most common cause of hypercalcemia, due to excess Parathyroid hormone (PTH) release by the parathyroid glands. Therefore, since both vitamin D and parathyroid hormone help manage calcium balance in the body it is beneficial to look at PTH as an indicator of bone health because vitamin D supplementation can also lower serum PTH which can lead to osteomalacia, bone loss, and increased risk of fracture.[15]
Excess Vitamin D And Hypothyroidism
The thyroid gland is typically the first victim of excess 1,25-D because it will park in the thyroid receptor. A poorly functioning thyroid is often the result T4 hormone not converting into the bioactive hormone, T3, but instead converting into the inactive rT3 (reverse tri-iodothyronine) hormone. As rT3 levels increase, T3 levels fall (hypothyroidism) metabolism and body temp decreases, and various enzymes fail to function properly. In addition, elevated cortisol due to adrenal dysfunction can contribute to this faulty conversion.
The pattern to select for inactive thyroid hormone, rT3, at the receptor site is the same pattern for vitamin D metabolism. According to several studies, vitamin D-deficiency is linked to changes in the VDR, vitamin D-binding protein, and enzymes when thyroid autoantibodies are present. Different alleles are affected between Hashimoto’s and Graves and also between different cultural groups.[16] Both thyroid hormone and vitamin D hormone metabolism appear to downregulate in response to inflammation caused by a shift in our microbes at the level of the gut.
Vitamin D and Cancer
Research shows a link between high levels of bioavailable, circulating inactive 25-D and pancreatic cancer risk. One study in the March 2012 Journal of Cancer Research suggests it may be valuable to look at levels of D-binding protein (DBP) and inactive 25-D in determining cancer risk since it is thought that higher DBP concentrations may sequester more 25-D and reduce free 25-D bioavailability. All tolled, about 1% of 25-D circulates freely while 10-15% is bound to albumin – it is this combined fraction of vitamin D that is considered bioavailable or “free25-D.” [17] Note: albumin in vaccines may further interfere with levels of free 2-5-D.
Another parameter to monitor is the nagalase enzyme. This enzyme sabotages vitamin D-binding protein, also known as GcMAF, or Gc. Gc is converted into GcMAF, by a combination of B and T immune cells. GCMAF then activates the immune system by its binding to macrophages and vitamin D. Cancer cells and viruses release biotoxins, including the nagalase enzyme which splits apart the protein Gc-MAF.
When nagalase splits Gc-MAF, it binds to the Gc protein and thereby prevents macrophages, and vitamin D from binding to it. When Gc protein cannot be converted to GcMAF the entire immune system is disabled. Nagalase spreads with impunity. One nagalase enzyme molecule can destroy a large quantity of GcMAF molecules. With no natural enemies – except radiation and chemotherapy – which destroy the immune system, only the addition of GcMAF protein in the body can reactivate the immune system.
Nagalase enzyme can also be used as a tool to track the rise or fall of cancer in the body. Many doctors who understand this relationship have successfully used GcMAF therapy over a six month course to reverse cancer and autoimmune disease. The protocol recommends 100 ng GcMAF intramuscular injections. Monthly Nagalase level tests follow the Nagalase level as it reverts back to baseline. Allopathic medicine has yet to embrace nagalase as a measure of cancer reversal since they are forever looking for an elusive “cure.” Measuring nagalase enzyme in patients with prostate cancer administered GcMAF immunotherapy showed complete tumor reversal and no recurrence for seven years.
 Part IV: Testing, Therapies, Treatment
Part IV: Testing, Therapies, Treatment
As long as medicine continues to rely on dried blood analysis, vs. live blood analysis, it is beneficial to look at both biomarkers in the blood; the active and inactive forms of vitamin D, as well as vitamin D binding protein, kidney function tests, and other hormone testing (Parathryoid hormone, thyroid hormone, antibodies, enzymes, etc).
- 1, 25 (OH) Active
- 25 (OH) Inactive
- vitamin D binding protein
- Parathyroid hormone and other hormones
Testing only for the inactive form does not reveal the big picture. If inactive 25-D preferentially binds to VDR receptor sites, there is not enough information to know if there is a conversion problem or if active 1,25D is blocking other hormonal receptors based on artificial supplementation of vitamin D.
Autoimmune Disease (Th1)
Th1 is the humoral wing of the immune system. Th2 is the B cell, or antibody wing of the immune system. The T-helper Type 1 (Th1) immune response, or autoimmunity, is often defined as one which generates significant quantities of the cytokine Interferon-gamma. Patients with Th1 inflammation, who have not been supplementing with vitamin D, often have a low level of 25-D while the level of 1,25-D is high. Testing only 25-D, as is usually done, may result in a false diagnosis of vitamin D deficiency.
Trevor Marshall suggests that all autoimmune diseases are due to a correctable defect in innate immunity from a dysregulation of vitamin D. 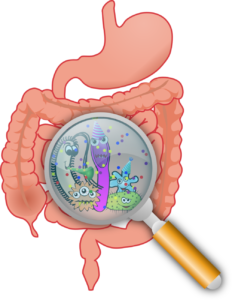
I disagree that Th1 patients each have different illnesses. I have seen no data to confirm this. Everything I see is that all the Th1 diagnoses spring from a common pathogenesis, a special adaptation of intra-phagocytic bacteria which allows them to evade phagocytosis by stimulating a Th1 response in the parasitized phagocytes.
I personally believe that ALL the Th1 diseases result from the same bacterial pathogenesis. This belief is grounded in my understanding of how the bacteria directly drive the phagocytic biochemistry, causing the Th1 cytokine release. IMO, it is important for everybody to stop thinking about these Th1 syndromes as being separate and discrete diagnoses. IMO, all Th1 illness has a common pathogenesis, only the mix of symptoms varies from person to person, depending on bacterial species present, and the sequence of infection/coinfection. – T. Marshall from article
Yet science is reluctant to let go of their vitamin D2 therapies. A 2022 study in The British Medical Journal claims that 2000 iu/day of vitamin D reduced the incidence of autoimmune disease by 22% over 5 years in people with autoimmune disease. This includes “all incident autoimmune diseases”: rheumatoid arthritis, polymyalgia, rheumatica, autoimmune thyroid disease, systemic lupus, psoriasis, and others [18]. However, there is never an indication that a full reversal of autoimmune is ever possible. Medical science would rather ignore that vitamin D is a steroid hormone and keep people suspended in autoimmunity indefinitely. Adding any synthetic hormone to the body naturally cuts off communication between the glands, especially when vitamin D blocks the VDR and thyroid cell receptors. As someone who personally reversed autoimmune thyroiditis using Nature’s tools, in less than one year, without vitamin D supplementation, why would anyone want to prolong disease if there is another way?
Low levels of 1,25 (active) D may also indicate kidney dysfunction if the kidneys are unable to activate inactive 25-D to active 1,25-D. While most people assume a high amount of 1, 25-D is best, high levels may indicate parathyroid disease, sarcoidosis, rheumatoid arthritis, fibromyalgia, Lyme disease and other inflammatory autoimmune conditions.
Therapies and Treatments
Prevention and treatment of autoimmune conditions and cancer in the medical community uses a patent for biologically active vitamin D compounds in combination with at least one other immunomodulatory compound such as interleukin-10, interleukin-4, or a TNF.alpha. inhibitor. The patented drug Benicar is used as the core drug in the Marshall Protocol, developed by Trevor Marshall. Similarly, patented L-carnosine salt used to treat and prevent inflammatory bowel disease. However, be aware that these patented drugs may have a limited effect due to the side effects of any drug therapy, which are not natural to the body and ultimately cause congestion in the blood and various organs.
The Natural Option
Rosemary appears to be the natural option to Benicar because it contains L- carnosine, which is a powerful VDR antagonist. L-carnosine in rosemary, sage, oregano, and other herbs acts as an anti-oxidant, chelator of copper cations, prevents protein glycation, is a pH buffer, and has a rejuvenating effect. Meat is the natural dietary source of carnosine.
Here is 1,25D as it docks into the VDR with the superimposition of carnosic acid (color) contained in rosemary and sage. A pure source of Rosemary can be found here.
Variations in polymorphisms in the VDR may alert the need for additional nutritional support. For instance, the defect at the gene position VDR Fok + can impact vitamin D levels. Research shows that supplementing vitamin D may be beneficial. Sage and rosemary support vitamin D receptors. It may be necessary to support the pancreas when having a VDR Fok + mutation using vitamin and digestive/pancreatic enzymes.
It’s Epigenetics
Secosteroid “vitamin” D is an epigenetic innovator. Without a full understanding of the “sunshine vitamin,” we must be careful in promoting solutions that may actually be driving disease manifestation higher in the population.
 Like Nature, our bodies are homeostatically regulated, meaning that our intricate metabolic system through the cells compensate for environmental changes by making the appropriate internal changes in order to restore balance. Just as body temperature, blood glucose, and countless other internal variables are self-regulated, so too, is vitamin D metabolism. And these cellular changes are driven by our innate and adaptive immune systems which are driven at the level of our cells, through the wisdom of the body itself. Science breaks down this wisdom into receptors such as VDR, CD-R, and cytokines that summon and cause the creation of our macrophages to defend health.
Like Nature, our bodies are homeostatically regulated, meaning that our intricate metabolic system through the cells compensate for environmental changes by making the appropriate internal changes in order to restore balance. Just as body temperature, blood glucose, and countless other internal variables are self-regulated, so too, is vitamin D metabolism. And these cellular changes are driven by our innate and adaptive immune systems which are driven at the level of our cells, through the wisdom of the body itself. Science breaks down this wisdom into receptors such as VDR, CD-R, and cytokines that summon and cause the creation of our macrophages to defend health.
The alternate hypothesis – that vitamin D serum levels are modified by disease processes – is far more compelling than the currently accepted ‘vitamin’ ideology – that the lower levels observed in sick individuals are indicative of a nutritional deficiency.
We must address the Candida and Lyme disease that underlies D-deficiency if the body is to rebalance itself. For Lyme disease or any disease to manifest, they depend on the conditions of the body’s terrain (pH, nutritional status, toxicity). The imbalance of normal flora results from an acidic gut environment that results from an acidic intestine that results from leaky gut. An excess of acid in the body and an acidic intestinal tract can come from decreased liver function and an accumulation of toxins from food, air, water, amalgams, vaccines, drugs, and a poor diet, once known as toxemia.
If our bugs tell us anything, it is to remind us that the best we can do for the body is to provide it the tools of Nature, starting with being out in nature. Sunshine is the best remedy for vitamin D balance.
Our bodies also require the right fuel from whole, fresh raw, fermented, pastured, healing foods, foods as close to the earth as possible. Foods and herbs in their original packages, naturally balanced in nutrients (fish liver oils), live foods, rich vitamins, minerals, fats, carbohydrates, proteins, and bacteria. Foods that heal the gut (bone broths). We must select foods, and food-based supplements, for their hermetic ability to modulate optimal levels of vitamin D and other hormones in the body. Of these, cod liver oil, preserved naturally with rosemary oil, is an excellent form that the body naturally utilizes.
Avoid EMFs
It is important to be aware of growing dangers in the environment, namely; increased level metals, chemicals, and electromagnetic fields (EMFs), which create an acidic body. EMFs produce rapid increases in intracellular calcium levels. Levels of 4G and 5G frequencies also increase the levels of mycotoxin of molds and yeasts. Electromagnetic fields are millions of times higher than ten yeast ago. These frequencies disrupt communications inside the cells to affect the immune system which cause increased rates of disease. Avoiding these dangers can go far toward reducing disease rates when artificial hormone supplementation offers little to no decrease in chronic disease rates.
Along with a nutrient-dense diet, adequate rest, knowing the body’s natural affinity for plants, and avoiding EMFs, these are the best ways to stay healthy. To ensure optimal vitamin D levels is to follow the sun and allow your body’s wisdom to lead the way to health.
*Special thanks to Jim Stephenson Jr for the invaluable assistance in collecting the studies.
 References
References
[1] Marshall, Trevor G. “Vitamin D Discovery Outpaces FDA Decision Making.” Bioessays BioEssays 30.2 (2008): 173-82. Web. Feb. 2008. <http://www.ncbi.nlm.nih.gov/pubmed/18200565>.
[2] Wagner, Carol L., Thomas C. Hulsey, Deanna Fanning, Myla Ebeling, and Bruce W. Hollis. “High-Dose Vitamin D 3 Supplementation in a Cohort of Breastfeeding Mothers and Their Infants: A 6-Month Follow-Up Pilot Study.” Breastfeeding Medicine 1.2 (2006): 59-70. Web. 2 Nov. 2006. <http://www.direct-ms.org/pdf/VitDGenScience/Hollis%20breastfeeding%20D%20level%2007.pdf>.
[2.5] Arya, V., Bhambri, R., Godbole, M.M. et al. Vitamin D status and its relationship with bone mineral density in healthy Asian Indians. Osteoporos Int 15, 56–61 (2004). https://doi.org/10.1007/s00198-003-1491-3
[3] Powe, Camille E., Michele K. Evans, Julia Wenger, and Alan B. Zonderman. “Vitamin D–Binding Protein and Vitamin D Status of Black Americans and White Americans.” New England Journal of Medicine N Engl J Med 369.21 (2013): 1991-2000. Web. 2013. <http://www.ncbi.nlm.nih.gov/pubmed/24256378>.
[4] Batai, Ken, Adam B. Murphy, Ebony Shah, and Maria Ruden. “Common Vitamin D Pathway Gene Variants Reveal Contrasting Effects on Serum Vitamin D Levels in African Americans and European Americans.” Hum Genet Human Genetics 133.11 (2014): 1395-405. Web. Nov. 2014. <http://link.springer.com/article/10.1007/s00439-014-1472-y/fulltext.html>.
[5] Proal, Amy. “Study Finds That Healthy Indian Hospital Workers Display Low Levels of Vitamin D despite Adequate Sun Exposure, Providing Support for Marshall’s Model of Vitamin D Metabolism.” Study Finds That Healthy Indian Hospital Workers Display Low Levels of Vitamin D despite Adequate Sun Exposure, Providing Support for Marshall’s Model of Vitamin D Metabolism. Http://bacteriality.com/, 20 June 2008. Web. 06 Feb. 2016. <http://bacteriality.com/2008/06/indian/>.
[5.5] Albert PJ, Proal AD, Marshall TG. Vitamin D: the alternative hypothesis. Autoimmun Rev. 2009 Jul;8(8):639-44. doi: 10.1016/j.autrev.2009.02.011. Epub 2009 Feb 12. PMID: 19393200.[6] Marshall, Trevor G. “Vitamin D Discovery Outpaces FDA Decision Making.” Bioessays BioEssays 30.2 (2008): 173-82. Web. 30 Feb. 2008. <http://www.ncbi.nlm.nih.gov/pubmed/18200565>.
[7] Waterhouse, Joyce C., Thomas H. Perez, and Paul J. Albert. “Reversing Bacteria-induced Vitamin D Receptor Dysfunction Is Key to Autoimmune Disease.” Annals of the New York Academy of Sciences 1173.1 (2009): 757-65. Web. Sept. 2009. <http://www.ncbi.nlm.nih.gov/pubmed/19758226>.
[8] Nilsson, Kenneth, Carl Påhlson, Agneta Lukinius, and Lars Eriksson. “Presence of Rickettsia Helvetica in Granulomatous Tissue from Patients with Sarcoidosis.” The Journal of Infectious Diseases J INFECT DIS 185.8 (2002): 1128-138. Web. 15 Apr. 2002. <http://www.ncbi.nlm.nih.gov/pubmed/11930323>.
[9] Marshall, Trevor G., and Frances E. Marshall. “Sarcoidosis Succumbs to Antibiotics—implications for Autoimmune Disease.” Autoimmunity Reviews 3.4 (2004): 295-300. Web. 3 June 2004. <http://www.ncbi.nlm.nih.gov/pubmed/15246025>.
[10] Ibid. Waterhouse, et al. “Reversing Bacteria-induced Vitamin D Receptor Dysfunction Is Key to Autoimmune Disease.” Sept. 2009.
[11] Lim, Joan Hui Juan, Sharada Ravikumar, Yan-Ming Wang, and Thomas Paulraj Thamboo. “Bimodal Influence of Vitamin D in Host Response to Systemic Candida Infection—Vitamin D Dose Matters.” Journal of Infectious Diseases J Infect Dis. 212.4 (2015): 635-44. Web. 2015. <http://www.ncbi.nlm.nih.gov/pubmed/25612733>.
[12] Amer, Muhammad, and Rehan Qayyum. “Relation Between Serum 25-Hydroxyvitamin D and C-Reactive Protein in Asymptomatic Adults (From the Continuous National Health and Nutrition Examination Survey 2001 to 2006).” The American Journal of Cardiology 109.2 (2012): 226-30. Web. 2012. <http://www.ncbi.nlm.nih.gov/pubmed/21996139>.
[13] Amer, Muhammad, and Rehan Qayyum. “The Relationship Between 25-Hydroxyvitamin D and Homocysteine in Asymptomatic Adults.” The Journal of Clinical Endocrinology & Metabolism 99.2 (2014): 633-38. Web. 2105. <http://www.ncbi.nlm.nih.gov/pubmed/24276459>.
[14] Warrell RP Jr: Metabolic emergencies. In: DeVita VT Jr, Hellman S, Rosenberg SA, eds.: Cancer: Principles and Practice of Oncology. 5th ed. Philadelphia, Pa: Lippincott-Raven Publishers, 1997, pp 2486-93.
[15] Malabanan, A., Ie Veronikis, and Mf Holick. “Redefining Vitamin D Insufficiency.” The Lancet 351.9105 (1998): 805-06. Web. 14 Mar. 1998. <http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(05)78933-9/abstract>.
[16] Kivity, Shaye, Nancy Agmon-Levin, Michael Zisappl, and Yinon Shapira. “Vitamin D and Autoimmune Thyroid Diseases.” Cell Mol Immunol Cellular and Molecular Immunology 8.3 (2011): 243-47. Web. Jan. 2011. <http://www.nature.com/cmi/journal/v8/n3/full/cmi201073a.html>.
[17] Weinstein, Stephanie J., et al. “Impact of Circulating Vitamin D Binding Protein Levels on the Association between 25-Hydroxyvitamin D and Pancreatic Cancer Risk: A Nested Case–Control Study.” Cancer Res (2012) 72 (5): 1190–1198., Mar 1 2012, doi:https://doi.org/10.1158/0008-5472.CAN-11-2950.
[18] Hahn J, Cook NR, Alexander EK, Friedman S, Walter J, Bubes V, Kotler G, Lee IM, Manson JE, Costenbader KH. Vitamin D and marine omega 3 fatty acid supplementation and incident autoimmune disease: VITAL randomized controlled trial. BMJ. 2022 Jan 26;376:e066452. doi: 10.1136/bmj-2021-066452. PMID: 35082139; PMCID: PMC8791065.